Bed Blocking in the NHS and Why it’s a Problem
4 minute read | 03/08/2023

Bed blocking is a significant challenge for the NHS, where medically fit patients remain in hospital beds, causing strain on resources and increased costs. However, technology offers a powerful solution to alleviate this issue and transform healthcare delivery.
Learn more about it below.
Understanding bed blocking
Bed blocking can result from various factors, including delays in arranging social care, difficulties in finding suitable residential care facilities, or inadequate community support for patients who need to be discharged. It can also be affected by delayed discharge. This bottleneck situation not only disrupts hospital operations but also adversely affects patients' health outcomes.
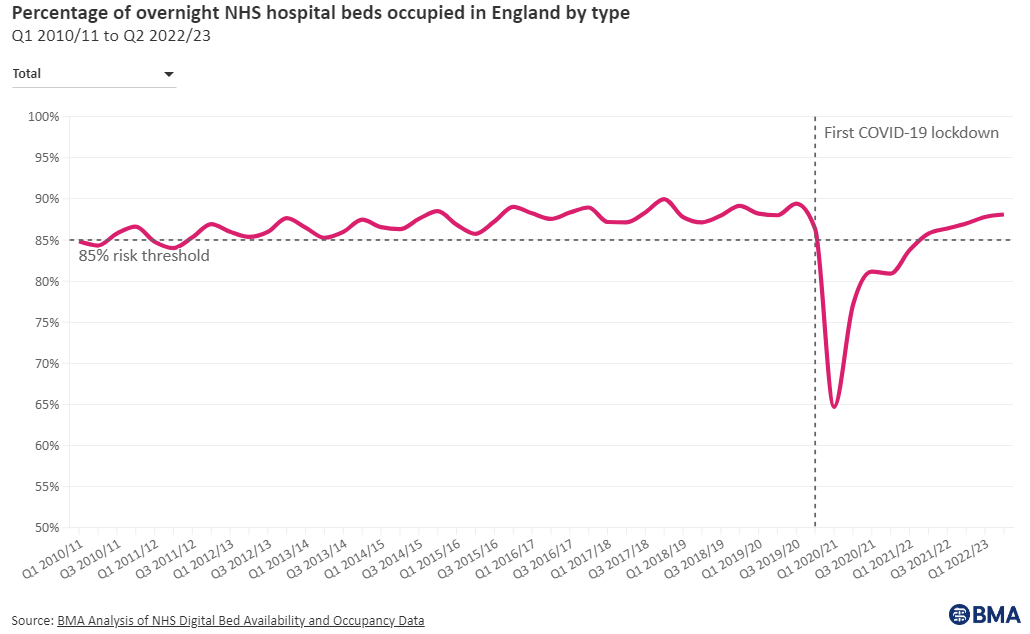
The Chief Executive of NHS Providers, Chris Hopson said "Evidence clearly shows that hospitals work most safely and effectively at bed occupancy levels no higher than 85%." as stated in NHS Providers.
The average occupancy rate for all beds open overnight during Quarter 4 of 2022/23 stood at 89.8%, surpassing the safety benchmark of 85%. This persistent trend of exceeding the benchmark since 2011 calls for immediate action to improve the situation and prevent further strain on the NHS.
4 Impacts of bed blocking
- Strained healthcare resources: When beds are occupied by patients who no longer require hospital care, there is a reduced capacity to admit new patients promptly, leading to longer waiting times and compromising the quality of care provided.
- Increased costs: The longer patients remain in hospital beds unnecessarily, the higher the financial burden on the NHS. Bed blocking contributes to escalating healthcare costs, ultimately affecting the healthcare budget.
- Adverse Health Outcomes: Extended stays in hospitals increase the risk of hospital-acquired infections, functional decline, and psychological distress for patients. It is vital to transition patients to appropriate care settings as soon as medically feasible.
- Staff Burnout: Hospital staff face additional challenges when dealing with overcrowded facilities and limited resources. This situation can lead to increased stress and burnout among healthcare professionals.
How to leverage apps for a solution
Technology has the potential to transform healthcare and offer innovative solutions to address bed blocking. Apps at the bedside can play a particularly important role by facilitating streamlined communication, creating efficient care coordination, and empowering patients and their families to actively participate in the discharge process.
- Enhanced communication and collaboration: Bedside apps streamline communication between healthcare professionals, improving coordination and reducing discharge delays.
- Real-time bed management: Bedside apps can provide real-time information about bed availability in various units or facilities within the hospital. This enables medical staff to quickly identify and allocate appropriate beds for incoming patients, minimising waiting times and preventing unnecessary bed occupancy.
- Integration with Electronic Health Records (EHRs): Integrating bedside apps with the hospital's EHR system allows healthcare providers to access up-to-date patient information, medical history, and test results. This comprehensive view of the patient's health status aids in making informed decisions about their discharge eligibility.

- Patient and family engagement: Bedside apps can empower patients and their families by providing them with access to further care resources. Companies like Autumna make it easier to find further care for the elderly. Informed patients are more likely to actively participate in their care planning and take necessary steps toward a timely discharge.
- Enhanced accessibility: Patient wellbeing is further aided by bedside access to room control as well as digital menus for meal ordering and shopping options for on-site services. This makes patients feel more comfortable and less restricted throughout the duration of their hospital stay.
All of these app capabilities can be delivered through SPARK Fusion®, a cutting-edge solution that is set to revolutionise patient care throughout the NHS. As an easy-to-use, app-based platform available via individually-tailored and customisable bedside devices, the possibilities for high-quality care increase while reducing the risk of bed blocking and readmission.
If SPARK Fusion® can contribute to even a 1% reduction in bed blocking, it would be a significant stride towards resolving the issue. While there may not be a single solution for bed blocking, SPARK Fusion® plays a crucial role in helping Trusts tackle this challenge.
Conclusion
The issue of bed blocking in the NHS is a complex and multi-faceted challenge that demands urgent attention. Embracing technology and integrating innovative solutions into healthcare practices can significantly alleviate bed blocking and its adverse effects on both patients and the healthcare system.
Investing in SPARK Fusion® is just one key action Trusts can take to accelerate their digital transformation while reducing the risk of bed blocking overall.
About the author
Rebecca O'Donovan
Becky is the Marketing Director at SPARK TSL, of whom she has worked for since 2012. She is responsible for high-level marketing strategy focusing on lead generation and aiding the vision of the business to ensure business growth.
More articles by the author
Related articles
.jpeg?width=386&height=180&name=AdobeStock_224040416-1%20(1).jpeg) Healthcare Industry
Healthcare Industry
How to Improve Hospital Patient Experience: What's Happened So Far
The desire to improve patient experience in hospitals isn’t a new concept — NHS Trusts have been ...
 Patient Experience
Patient Experience
How SPARK® Media is Helping UK Trusts Fight Patient Boredom
Isolation and boredom are issues that are sometimes overlooked on the hospital ward. During the pandemic, ...
 SPARK® Fusion
SPARK® Fusion
SPARK Fusion® Addresses NHS Challenges from Lord Darzi’s Report
In a recent independent investigation led by Lord Darzi, a number of pressing challenges currently faced by ...